The Siteman Blood Cancer Center, recognized internationally as a leader in innovative care, draws patients from across the U.S. and overseas. The center brings together the multidisciplinary expertise of WashU Medicine physicians who have a singular focus on treating blood cancers, including leukemia, lymphoma, multiple myeloma and myelodysplastic syndromes. They have long been at the forefront of transforming care and pushing the boundaries of what’s possible in managing these complex cancers.
Such progress stems from a solid foundation of research-informed care championed by leukemia expert John F. DiPersio, MD, PhD, the Virginia E. and Sam J. Golman Endowed Professor of Medicine, who led WashU Medicine’s Division of Oncology for more than 25 years. He was instrumental in establishing Siteman’s bone marrow transplant program for patients with blood cancers as one of the world’s best, and his ongoing research at WashU Medicine continues to move the field forward. In addition to developing novel cell-based immunotherapies, he is focused on alleviating graft-versus-host disease, a potentially deadly complication of bone marrow transplantation. His research has been fundamental to the FDA approval of medications to mobilize stem cells for transplant and the first drug approved to treat graft-versus-host disease.
WashU Medicine’s expertise in blood cancers runs deep. Physician-scientist Daniel C. Link, MD, also specializes in leukemia and conducts innovative research aimed at developing better treatments for blood cancer. He is deputy director of Siteman and director of the Division of Oncology. Link is a world leader in understanding hematopoiesis, the process by which different types of blood cells are formed and has helped develop WashU Medicine’s hematopoietic malignancy research program into one of the top such programs in the country. He also leads efforts aimed at boosting translational research and moving promising investigational treatments — developed at WashU Medicine — into clinical trials.
In addition to Link, the Alan A. and Edith L. Wolff Distinguished Professor of Medicine, the Siteman Blood Cancer Center is led by Amanda F. Cashen, MD, a professor of medicine and associate chief of the Hematologic Malignancies Program, and Brad S. Kahl, MD, a professor of medicine and director of the Lymphoma Program.

Patients with blood cancers who seek care at Siteman have access to the most advanced diagnostic techniques, the latest, most advanced treatments, including immunotherapies, and an array of clinical trials aimed at developing new, more effective treatments options.
“Our patients benefit from decades of outstanding clinical care and research led by WashU Medicine physicians and researchers at Siteman,” Cashen said. “This level of expertise also helps us recruit the brightest talents in blood cancer research and train a new generation of physicians and physician-scientists dedicated to further improving outcomes for patients.”
Patients receive expert care guided by the most advanced genetic tests available, including whole cancer genome sequencing for acute myeloid leukemia (AML) through the ChromoSeq test, developed by WashU Medicine physician-scientists and the first to be approved for reimbursement by the Centers for Medicare & Medicaid Services.
The Siteman Blood Cancer Center also has received a prestigious Specialized Program of Research Excellence (SPORE) in Leukemia grant from the National Cancer Institute — one of only two active Leukemia SPOREs in the country. The award funds research to develop the next generation of blood cancer therapeutics.
Stem cell transplants provide the possibility of a cure for some blood cell cancers and can only be performed at specialized centers. WashU Medicine physicians have performed more than 10,000 stem cell transplants at Siteman, making the cancer center one of the largest and most experienced bone marrow transplant programs in the country. “Very few institutions in the U.S. have the expertise and resources that WashU Medicine and BJC HealthCare bring together to care for patients at Siteman,” Cashen said. “For patients with blood cancers, we draw on our wealth of experience so they receive the very best care possible from a team that is absolutely committed to their care and supports patients every step of the way.”
Time, the ultimate gift
A New York doctor turns to WashU Medicine specialists at Siteman Cancer Center to treat the untreatable

Three years ago, a routine blood test showed that David B. Duggan, MD, had a high white-blood-cell count, suggesting an infection or illness of some sort.
“But I felt great,” recalled Duggan, a hematologist in New York. In his late 60s at the time, Duggan was active — he cycled, swam and worked on his 185-year-old farmhouse. He also taught medical students, conducted research and treated patients with leukemia, lymphoma and other blood cancers at the State University of New York Upstate Medical University in Syracuse, N.Y.
But within days of the blood test, Duggan received grim news. He had leukemia — specifically, T-cell prolymphocytic leukemia, or T-PLL, a rare, aggressive and often fatal cancer.
“Ironically, as a hematologist, I was quite familiar with T-PLL,” Duggan said. “I’ve treated patients with it, and it can progress quickly. Standard treatments aren’t terribly satisfying.” So, he started getting his affairs in order. He and his wife of 39 years, Lynn, took a two-week bucket-list trip to Ireland with family. He looked forward to being a part of major family events, including the birth of his first grandson, Colin, and the marriage of his youngest child. He stopped accepting new patients.
“My job was to be there for my patients,” he said. “I wasn’t sure if I’d be around.”
But then, Duggan discovered a phase 1 clinical trial 885 miles from home at Siteman Cancer Center. The international, multicenter trial is evaluating an innovative cellular immunotherapy that was developed by WashU Medicine’s John F. DiPersio, MD, PhD, the Virginia E. and Sam J. Golman Professor of Medicine, and his colleagues, fellow physician-scientists Geoffrey L. Uy, MD, co-leader of the Hematopoietic Development and Malignancy Program at Siteman and a professor of medicine in the oncology division; Michael Kramer, MD, PhD, WashU Medicine instructor in medicine; and Armin Ghobadi, MD, clinical director of the Center for Gene and Cellular Therapy and a professor of medicine in the oncology division at WashU Medicine.
The clinical trial is partly funded by Wugen, a startup cofounded by DiPersio, who also directs WashU Medicine’s Center for Gene and Cellular Immunotherapy at Siteman. The company — which is developing several lines of cell-based immunotherapies for various cancers — was cofounded by WashU Medicine physician-scientist Todd Fehniger, MD, PhD, co-leader of the Hematopoietic Development and Malignancy Program at Siteman and a professor of medicine in the division of oncology; Matthew Cooper, PhD, a former faculty member and Wugen’s chief scientific officer; and Melissa Berrien-Elliott, PhD, a former postdoc in Fehniger’s lab.
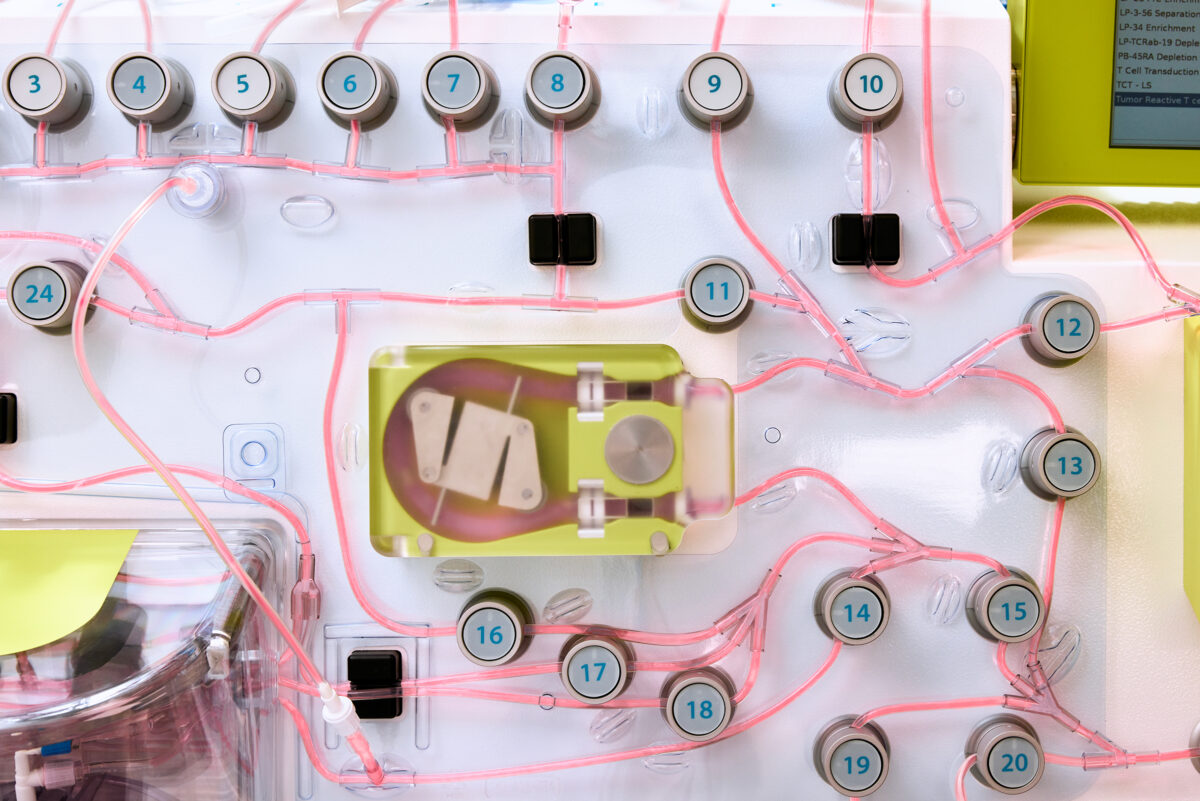
The trial involves CAR T-cell therapy, a type of cellular immunotherapy that uses genetically modified T cells to attack cancer cells. This particular CAR T-cell therapy is unique in that it is genetically engineered to attack T cell cancers, such as Duggan’s, rather than B cell cancers, the typical target of CAR T-cell therapies. But using genetically modified T cells to kill and eliminate the cancerous T cells is tricky, because the modified T cells risk mistaking themselves for the cancer and succumbing to friendly fire rather than eliminating the leukemia.
A second genetic modification helps overcome this challenge by eliminating the T cells’ ability to target one another, which also stops the cells from attacking the body’s healthy tissues, preventing a life-threatening side effect of treatment called graft-versus-host disease. These modifications further allow the therapeutic T cells to be collected from any healthy donor without concern about finding someone with an immune system match, which can take time and delay treatment against an aggressive disease.
Using the novel CAR T-cell therapy, Ghobadi administered the infusion to Duggan in early 2024. “He had a beautiful expansion of CAR T cells circulating throughout his body,” Ghobadi said. “It eventually led to the elimination of his malignant T cells, basically ridding the body of leukemia.”
In addition to Duggan, other patients who have received the CAR T-cell therapy have gone into remission, Ghobadi said. “The trial has introduced a new and exciting opportunity for treating patients who otherwise lacked other options.”
“As a doctor, I understand death,” Duggan said. “After my diagnosis, I was afraid I had little time left. But Siteman has given me access to WashU Medicine oncologists who are international leaders in their fields as well as this innovative clinical trial that’s granted me time. I am grateful because, boy, I sure enjoy living.”
“Boot camp” for cancer fighters
A donor’s or patient’s natural killer cells are “trained” using chemical signals to make them even better cancer fighters for the patient.
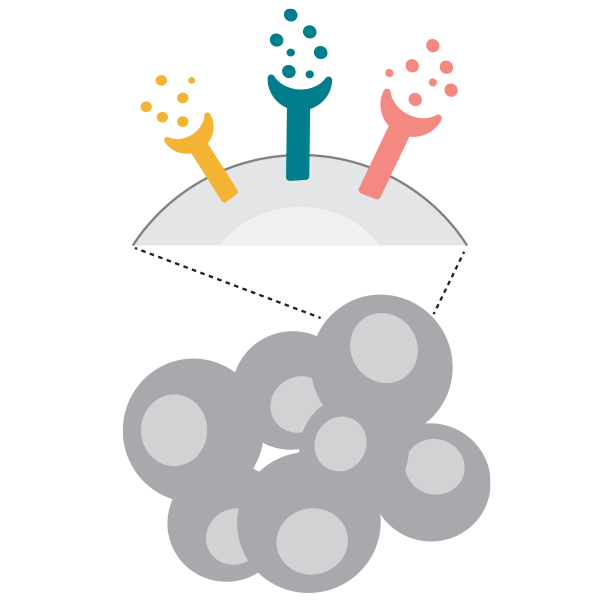
Natural Killer (NK) Cells
NK cells have an innate capacity to avoid “friendly fire” that allows them to attack only cancer cells and not harm the patient’s healthy cells. For some cancers, NK cells are engineered to express a new type of recognition that is specific for the targeted diseased cells.
The differentiated NK cells now “remember” their basic training, and once transplanted they will:
- Kill cancer cells
- Activate other immune cells
- Persist after transfer into a patient
Testing in clinical trials for:
- Leukemia
- Lymphoma
- Melanoma
Explore the extensive scope of cancer care and research.
Published in the Autumn 2024 issue


