Whether malignant or benign, a brain tumor is life-altering. Malignant tumors can spread and become deadly. And benign doesn’t mean harmless; benign tumors can cause serious problems such as paralysis, seizures and personality changes depending on which parts of the brain they affect.
“Brain tumors affect the fundamental attributes of people — their personality and behavior; their ability to move, speak, see, think — that are just such essential characteristics of a human being,” said neurosurgeon Albert H. Kim, MD, PhD, the founding director of the Brain Tumor Center at Siteman Cancer Center at Barnes-Jewish Hospital and Washington University School of Medicine. “To understand and treat brain tumors we have to attack them from different angles, and tailor therapy to each person.”

Personalized predictions
People with the neurofibromatosis type 1 (NF1) genetic disorder can develop tumors on nerves anywhere in the body, including in the brain. David H. Gutmann, MD, PhD, neurologist and director of the Washington University NF Center, discovered that the specific mutation a child is born with, neuronal activity and hormones all play roles in determining whether tumors develop and what problems they will cause. Based on these discoveries, Gutmann and data scientists Philip R.O. Payne, PhD, and Aditi Gupta, PhD, created risk-assessment models using advanced AI methods that can inform personalized approaches to management of each person with NF1.
“One of the biggest challenges in caring for children with NF1 is not being able to predict who might develop a brain tumor.”
— David H. Gutmann, MD, PhD
Zika’s silver lining
Zika virus made headlines worldwide in 2015 when it caused thousands of babies in Brazil to be born with tiny, misshapen brains. Neuro-oncologist Milan G. Chheda, MD, and virologist Michael S. Diamond, MD, PhD, aim to harness the virus’s infamous power to kill brain cells and direct it against brain cancers. They have shown that the virus can activate immune cells to destroy an aggressive brain cancer in mice, giving a powerful boost to an immunotherapy drug and sparking long-lasting immunological memory that can ward off tumor recurrence for at least 18 months.
Laser focus
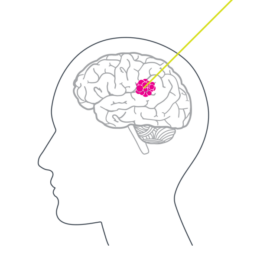
WashU Medicine neurosurgeons were among the first to use MRI-guided, high-intensity laser interstitial thermal therapy (LITT) to treat inoperable brain tumors. This minimally invasive technique uses lasers to heat and destroy tumors while leaving surrounding brain tissue undamaged. Neurosurgeon Albert H. Kim, MD, PhD, studies how to make laser therapy even more effective. He discovered that LITT temporarily opens the blood-brain barrier, potentially allowing chemotherapy drugs to mop up remaining cancerous cells, and stimulates the immune system, an opportunity to develop add-on immunotherapies. Alexander H. Stegh, PhD, research director of the Brain Tumor Center, targets tumors with a different approach, using nanotechnological platforms to manipulate the tumor’s genetic program and to arm the body’s immune system to fight brain cancers.
Breaking the barrier
Biomedical engineer Hong Chen, PhD, and neurosurgeon Eric C. Leuthardt, MD, pioneered sonobiopsy, which uses targeted ultrasound and microbubbles to temporarily disrupt the blood-brain barrier that normally shields the brain from harmful substances in the blood. This disruption allows RNA, DNA and proteins to flow from the brain into the blood where they can be detected and analyzed. “Sonobiopsies provide invaluable molecular and genetic information without the risks of brain surgery,” Leuthardt said. “It’s the third revolution in brain cancer diagnosis, after structural and functional brain imaging.”
Navigate the neurosciences
Continue exploring the extensive scope of neuroscience research conducted at WashU Medicine.
Published in the Winter 2023-24 issue