
A triumphal raise of the arms was an impossibility for Loren Schaller, who had suffered a knife attack, until peripheral nerve surgery restored her ability to perform such movements.
In May 2007, Loren Schaller was 15 when a prisoner mistakenly released from San Quentin randomly followed her into a San Francisco bakery, stabbing her five times. The knife sliced through her jugular vein, severing nerves in her neck. Bystanders’ quick actions helped saved her life, but Loren’s right arm was paralyzed from the shoulder to the wrist.
In the wake of the attack and heavy blood loss, the immediate focus was on keeping Loren alive. Doctors originally thought the paralysis would be short-lived, attributing it to a blood clot compressing her nerves. When the situation didn’t improve, a nerve study months later revealed the true problem.
Surgeons tried to reattach the cut nerves, but scar tissue made it impossible to find the nerve endings, and the effort was abandoned. The consensus: Loren would never move her arm again.
Loren’s parents, Linda and Tim Schaller, searched the country for a surgeon who could help restore movement in her arm, asking everyone they knew for possible leads.
Eventually, they came across an article in U.S News & World Report. Part of a series titled “Medical Mavericks,” the story highlighted the peripheral nerve work of Washington University surgeon Susan E. Mackinnon, MD.
Desperate for answers, the family soon was on a plane to St. Louis. Mackinnon advocated for nerve transfer, a procedure that, at the time, only a handful of U.S. surgeons was capable of performing. To do this, Mackinnon would reroute the circuit — connecting a functioning but redundant nerve in the upper arm to another more crucial nerve that had been severely damaged.
“After seeing Dr. Mackinnon, we finally had hope,” Linda Schaller recalled.
Mackinnon, chief of the Division of Plastic and Reconstructive Surgery and the Sydney M. Shoenberg Jr. and Robert H. Shoenberg Professor of Surgery, long has been in the business of hope.
Hundreds of thousands of people suffer debilitating nerve injuries every year from car wrecks, household mishaps and freak accidents. In a split second, peripheral nerves — the “electrical” wires connecting muscles to the brain and spinal cord — can be shredded or torn, rendering limbs forever lifeless. More than 25 years ago, Mackinnon adopted nerve surgery as her life’s work, and she has continued to push the envelope, exploring new ways to help patients regain some independence.
Nearly a decade since the attack, Loren has recovered remarkably. A 2014 UCLA graduate, she now works as a costume production assistant on ABC’s upcoming eight-part miniseries “When We Rise.” It’s a labor-intensive job; fortunately for Loren, she now has the ability to raise both arms above her head. “She (Mackinnon) rewired me,” Loren said with a smile.
Her parents, award-winning filmmakers, since have produced a documentary on Mackinnon called “A Spark of Nerve,” which premiered last November at the St. Louis International Film Festival. (View “A Spark of Nerve.” Access may be limited to devices connected to the Washington University School of Medicine network. Universities may request access via Kanopy Streaming. Learn more about the film project.)

At the St. Louis premiere of “A Spark of Nerve,” from left to right: Loren Schaller; her mother, Linda Schaller; music composer Fred Story; Loren’s father, Tim Schaller; and surgeon Susan Mackinnon, MD. Said Linda Schaller: “We made the film because we wanted others to know that there is hope.”
Taking small steps
In the world of peripheral nerve surgery, Mackinnon has trailblazed a unique niche. Although the Canadian-born Mackinnon started out in general and plastic surgery, she began working closely with neurosurgeon Alan Hudson, who was interested in nerve regrowth. In 1988, they performed the world’s first successful nerve transplant at Toronto’s St. Michael’s Hospital. Using nerves from a cadaver, the breakthrough restored movement to a nine-year-old boy’s injured leg.
Since joining the medical school faculty in 1991, Mackinnon has taken “incremental, small steps,” expanding upon those early techniques — moving from nerve grafting to nerve transplantation to nerve transfer — all while building a comprehensive nerve care center. The school’s Center for Nerve Injury and Paralysis is considered among the country’s most innovative.
The team includes several plastic and reconstructive surgeons dedicated to peripheral nerve injury repair, such as Thomas H. Tung, MD; Ida K. Fox, MD; Grant M. Kleiber, MD; Amy M. Moore, MD; and Alison K. Snyder-Warwick, MD; along with researcher Andrew Yee.
Tung and Moore were among the first to do nerve transfers for the treatment of lower-extremity nerve injury. Both are very active in basic science and clinical research related to nerve injury. Snyder-Warwick is the regional leader for reanimation after facial nerve paralysis. Kleiber is the newest member of the group who is knowledgeable about nerve transfer and other microsurgical techniques.
All work collaboratively to share information about unique and complicated cases. As Mackinnon explains, each surgery builds on the next.
A wiggle stuns the world
In 2008, Tom Wachtel, a 69-year-old Phoenix trauma surgeon, was driving to the hospital to perform emergency surgery when his car struck the median and flipped nose to end. Wachtel broke his neck and suffered a devastating spinal cord injury that left him a quadriplegic.
A couple years later, he sought out Mackinnon. Nerve transfer surgery never had been applied to a patient with a spinal cord injury and Mackinnon wasn’t sure it would work. Wachtel was willing to take the chance on the belief that others could learn from the experience.
For nine months post-surgery, they waited. That’s how long it took for the rerouted nerve to grow six inches toward Wachtel’s hand muscles.
One day he wiggled his finger and thumb. And Mackinnon? “I just went to the floor. I was so stunned and excited,” she said.
Wachtel had become the first quadriplegic to regain hand function via nerve transfer surgery, and the story made international headlines.
Eventually, Wachtel managed to eat a complete meal by himself and take control over other small, daily tasks. He gained enough independence to celebrate his 50th wedding anniversary at a Las Vegas restaurant. Two years into his recovery, he could catch a soccer ball.

All those who’ve had a successful nerve transfer surgery, raise your arms …. Tom Wachtel, MD, with Loren Schaller.
Mackinnon since has trained Fox as the surgical lead on nerve transfer procedures involving the cervical spinal cord. In total, 14 patients at Washington University Medical Center have undergone the procedure.
The technique has shown promising results for restoring function to select patients that otherwise would have been confined to a lifetime of hand paralysis, and ultimately laying the foundation for an emerging medical specialty.
“The world of nerve transfer surgery has been evolving for the last couple decades, in large part due to the efforts of Dr. Mackinnon,” said Gerald Wolff, MD, residency program director for the rehabilitation center at University of Ottawa in Canada, who was mentored by Mackinnon and Fox on the procedure.
The technique lays the foundation for an emerging medical specialty
“Dr. Mackinnon’s application of nerve transfers to restore upper-extremity function in tetraplegics (quadraplegics) is a pioneering technique. This is fast becoming the standard of care for treating those with peripheral nerve injuries,” he added.
In the U.S., approximately 250,000 people suffer from spinal cord injuries; more than half involve the neck. At this time, the nerve transfer surgery, however, is only effective in injuries affecting the lower neck.
The brain in conversation with the muscles
Seven vertebrae in the neck, denoted as C1 through C7, make up the cervical spinal cord. This nerve transfer surgery targets patients with injuries involving motor level function at the C6 or C7 vertebrae. It typically does not help patients who have lost all arm function due to higher injuries in the C1 through C5 levels.
In the procedure, Fox bypasses the spinal cord’s multitude of soft nerve bundles, which act as activity conduits to the brain, and instead redirects functioning nerves from a quadriplegic patient’s elbows or shoulders, connecting them to injured nerves going to areas of the hand or arm.
“In essence, the new nerve network reintroduces conversation between the brain and the muscles,” Fox said. “This permits patients to regain enough movement to perform tasks that encourage independence, such as drinking a glass of water or using the bathroom without assistance. These breakthroughs may seem small to most people but they are huge in terms of a patient’s quality of life.
“When you ask spinal cord injury patients what they miss most, what they want to improve their quality of life, hand function is No. 1 on the list,” Fox continued. “Having your hand lets you navigate the world.”

Following a paralyzing spinal injury, nerve transfer surgery performed by Ida Fox, MD, left, helped physician Michael Bavlsik, MD, resume activities such as grasping an otoscope.
Washington University primary care physician Michael Bavlsik, MD — a father of eight — agrees. Fox restored his ability to use his left hand following a 2012 car accident that left him a quadriplegic who moves about in a motorized wheelchair. Bavlsik now can grip an otoscope, reach out to get patient charts and drive. “I am extremely grateful for this surgery,” Bavlsik said.
Post-surgery, patients undergo extensive physical therapy to train the brain to recognize the new nerve signals, a process that takes up to two years.
Most patients say hand function would help restore quality of life
Fox engages in meticulous pre-surgical patient screening, spending hours assessing overall health and social support, among other factors. She works with a team of colleagues, including physical therapists, led by Lorna Kahn, PT, CHT; physiatrists, including Neringa Juknis, MD, and Rimma Ruvinskaya, MD; and neurologists, led by Craig Zaidman, MD.
Most important in the patient evaluation is the psychological component. “This trumps everything,” Fox said. “It is so vitally important. You have to set realistic expectations. This operation is not a cure. It’s not going to bring the patient back to pre-injury movement. It is incremental, but very real progress.”
This past fall, the Journal of Plastic and Reconstructive Surgery published a study led by Fox that assessed outcomes of nerve transfer surgery in nine cervical spinal cord-injury patients with upper-limb paralysis. Most patients reported improved hand and arm function.
Expanding training
Because so few surgeons perform spinal cord nerve transfers, quadriplegic patients from across the U.S. travel to the School of Medicine seeking its expertise. And Mackinnon and Fox are passionate about teaching these methods to surgeons far and wide.
The pair traveled to Ottawa in March 2015, supervising as Kirsty Usher Boyd, MD, a former surgical fellow at Washington University, became the first surgeon in Canada to perform the nerve transfer procedure on a quadriplegic patient, 44-year-old Tim Raglin. Eight years earlier, Raglin had dove off the dock of his family’s cottage — a jump he had made hundreds of times before, but this time water levels were unusually low and he struck the bottom.
Mackinnon and Fox guided Boyd through patient evaluation, delicate nerve topography, physiology and anatomy.
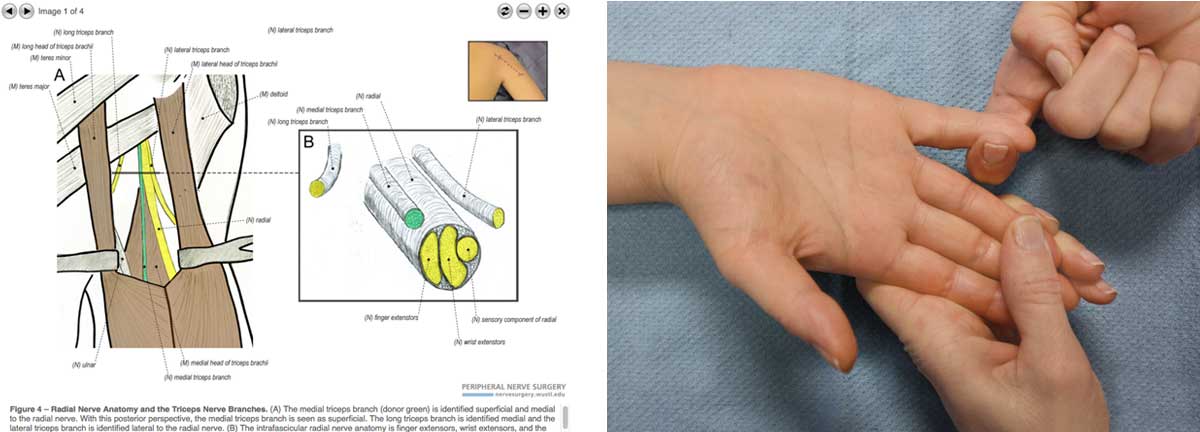
In another training initiative, the medical school’s plastic and reconstructive surgery division has launched a website, Peripheral Nerve Surgery: A Resource for Surgeons. The website offers step-by-step surgical videos on procedures ranging from simple nerve repairs to more complex injuries. “Every ‘recipe’ we have will go on there,” Mackinnon said.
For Mackinnon and Fox — standing on the forefront of these novel procedures — the hope is that more surgeons will embrace these adaptive techniques, restoring limbs and life to patients worldwide.
Site offers how-to for surgeons, perspective for patients
Sparked by the wars in Iraq and Afghanistan and initially geared toward military doctors, an open-access website now is an available tool for all surgeons and patients. The site provides step-by-step training videos and other learning resources for peripheral nerve surgeries.
Because of improvements in body armor, thousands of service men and women were surviving injuries that previously would have proven fatal, but returning home with debilitating peripheral nerve injuries. To better deal with this health-care crisis, the Henry M. Jackson Foundation for the Advancement of Military Medicine called for proposals. The Washington University team developed the site in response. Division team members respond to viewer questions and continually sharpen the website’s effectiveness as a teaching tool.
Published in the Summer 2016 issue


