A year and a half after the first COVID-19 shutdowns in the U.S. transformed life as we know it, the end to the pandemic is nowhere in sight. Masking and distancing can bring case numbers down, but at an economic and social cost many find intolerably high. Scientists developed fantastically effective vaccines in record time, but officials failed to get shots into arms fast enough to prevent a devastating fourth wave in the U.S.
For the physicians and scientists at the School of Medicine, reining in COVID-19 has been an ever-changing struggle. In the first, desperate months, they dove into the global race to find treatments, diagnostics and vaccines. Later, attention shifted toward understanding the long tail of COVID-19 symptoms, monitoring the threat of new virus variants, studying racial inequities and optimizing vaccination strategies.
Experts predict that mass vaccination eventually will end the pandemic but won’t eradicate the virus. We will just have to learn to live with it, they say. But the insights into human biology and behavior gleaned from this extraordinary time also will stay with us, informing medical care as we all adapt to the new normal.

The long tail of COVID-19
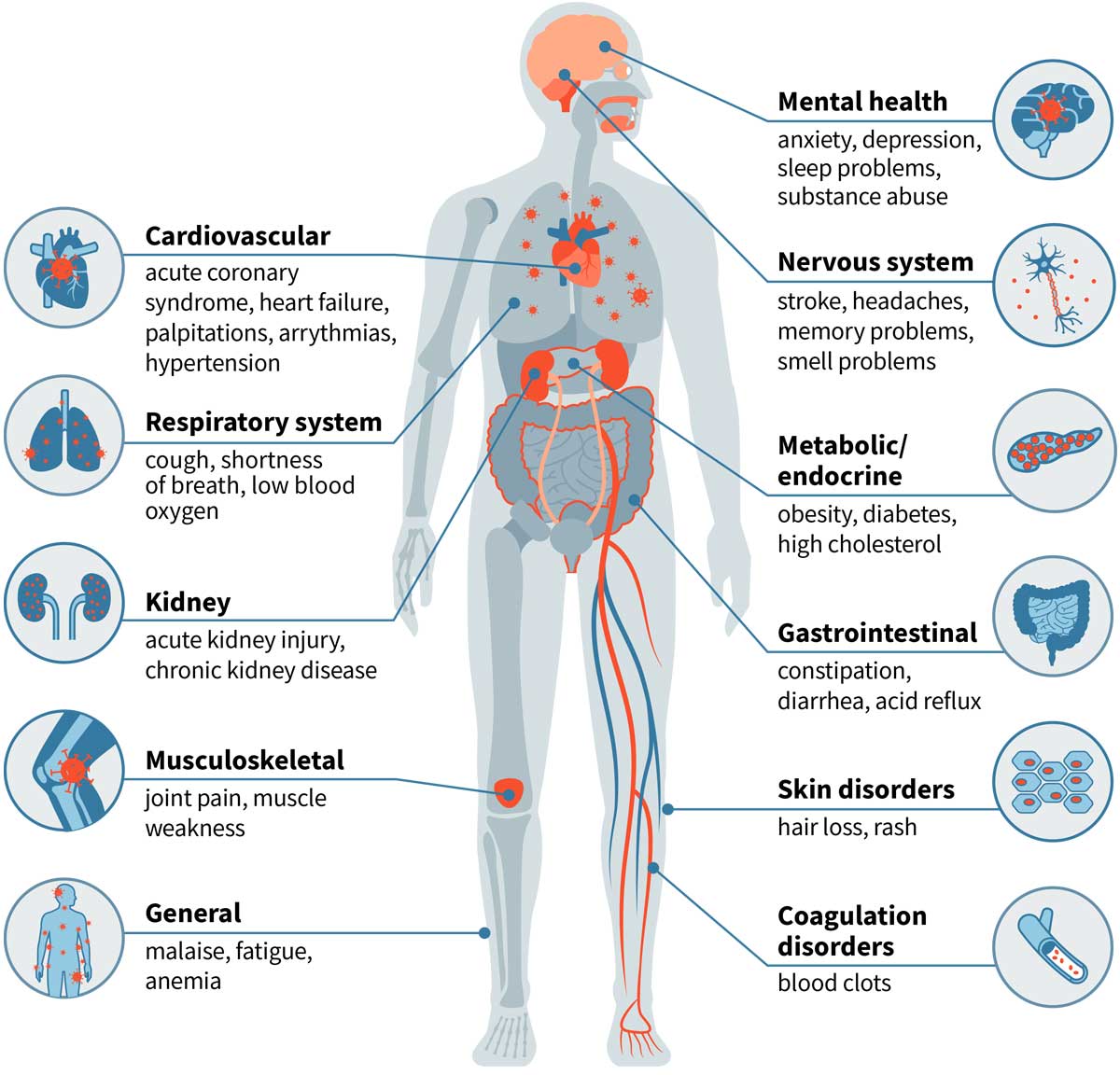
Some people survive COVID-19 but don’t fully recover for months, if at all. School of Medicine researchers are investigating why the effects of COVID-19 can linger long after the virus is gone.
Still at risk
Even people with mild cases of COVID-19 are at increased risk of death for months after the acute illness has passed, according to a study by Ziyad Al-Aly, MD, a kidney doctor who specializes in big data. By analyzing thousands of veterans’ health records, Al-Aly found that COVID-19 survivors face nearly a 60% higher chance of death from all causes in the six months after diagnosis. The higher risk of death was linked to persistent major health issues affecting nearly every organ system.

The vaccine race
With multiple COVID-19 vaccines available and the global vaccination effort underway, focus has shifted to understanding how well such vaccines work for special populations and creating better vaccines for current and future pandemics.

Closing the deal
Bringing this virus to heel requires not just having effective vaccines but getting those vaccines into the people who still need them, monitoring how long immunity lasts, and tracking the spread of new virus variants.

The new normal
When the pandemic recedes, the world will be different. Telemedicine may be here to stay, and possibly masking in winter, too. And the racial inequities laid bare by the pandemic may spur a reassessment of biases in medicine and a move toward better health for all.
Published in the Autumn 2021 issue