
Detached prosthetic limbs in pink and blue add flare to a colorless scene of Bunsen burners and beakers, microscopes and magnifiers, computers and chemicals sprawling inside the Minimally Invasive Surgery (MIS) Biomaterials Laboratory at Washington University School of Medicine.
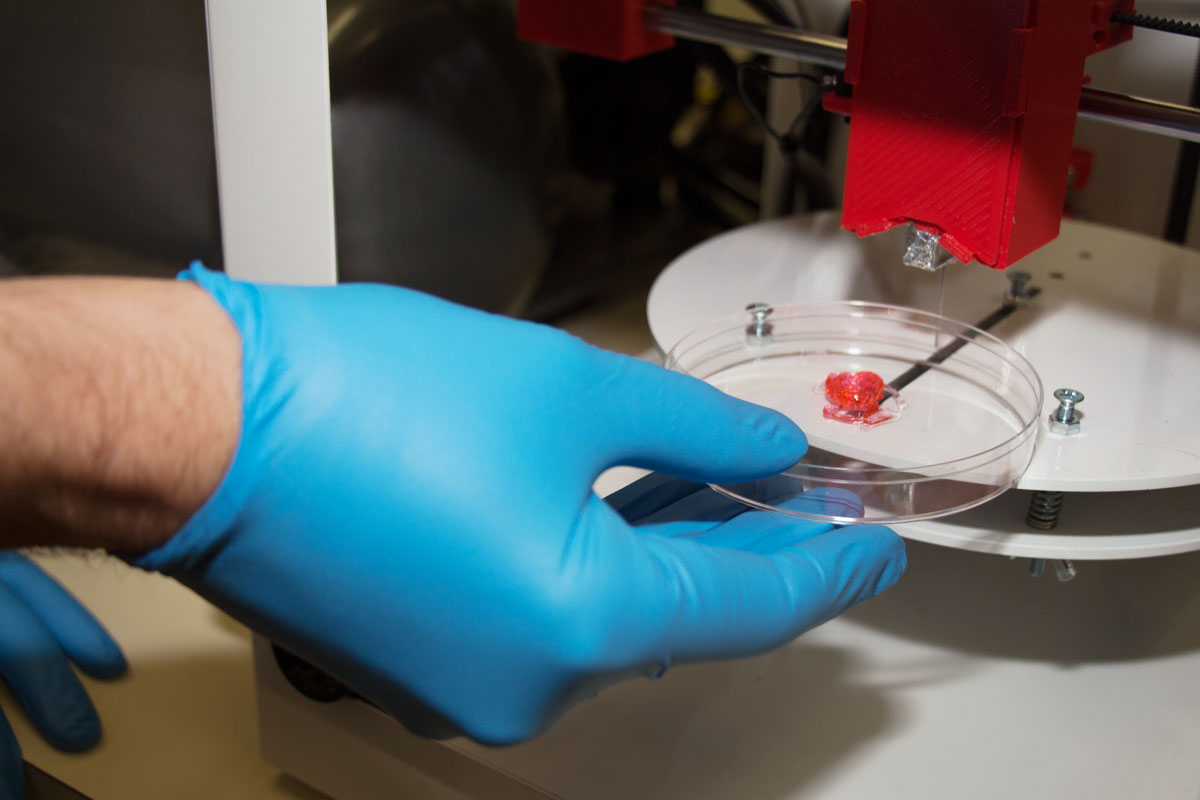
But the lab’s superstar — a desktop 3-D printer — appears nondescript, a big black box of a wallflower, a device resembling a microwave both in its appearance and in its revolutionary potential to transform an industry. The powerhouse prints three-dimensional body parts, including the prosthetic hands and arms in bubble-gum pink and baby-boy blue. The tool allows researchers to shape raw materials to meet specific health needs and, in the process, is heralding a new direction in patient care.
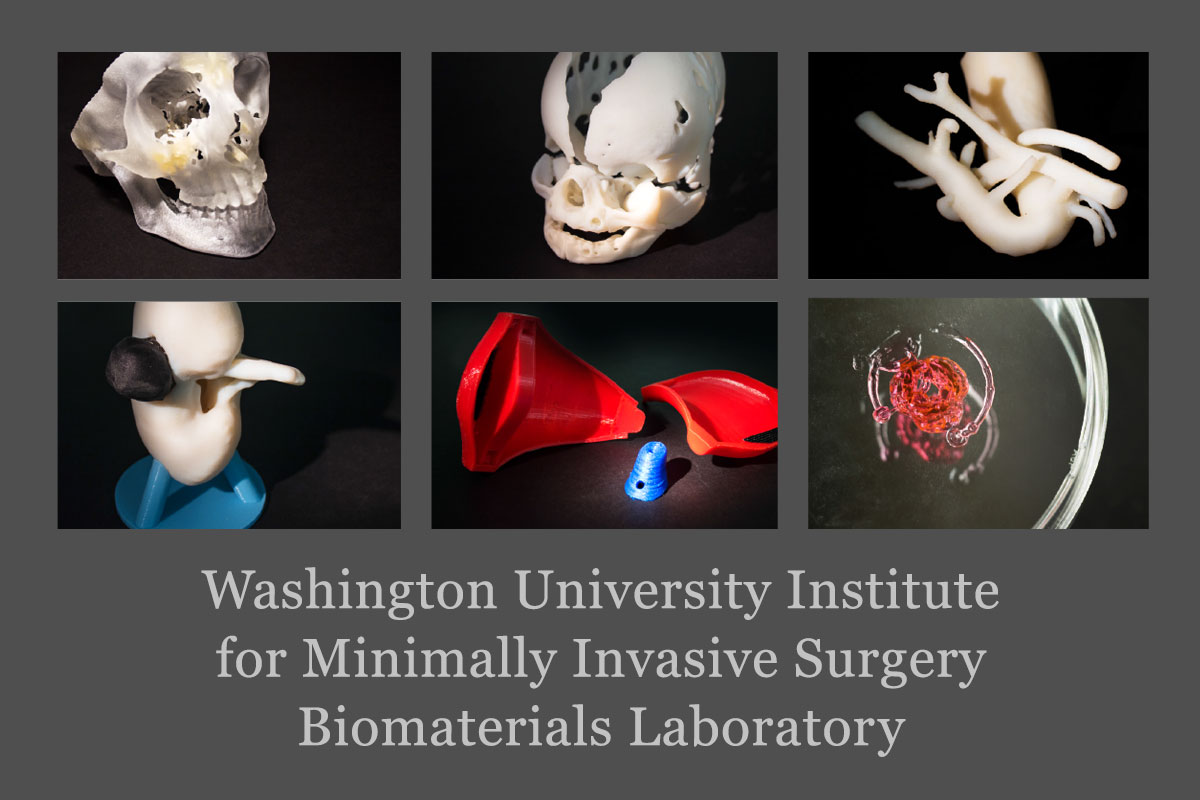
Globally, the medical industry is experimenting with 3-D printers to treat patients, tailor-making everything from skull fragments to fingers and teeth to heart valves and stents. Scientists, including those at the School of Medicine, also have ventured into the field of regenerative medicine by printing structures from living cells instead of inorganic materials. The ultimate goal in the medical field is to print a patient’s own cells, for instance, to regrow complex nerves after an injury or to create implantable organs for transplant patients that could eliminate waiting lists and organ rejection.
At the MIS lab, physicians, scientists and engineering students have carved a niche in 3-D printing: Producing prosthetic arms and hands for children who have lost limbs due to disease or accidental injury. The team’s efforts have attracted a lot of media attention since pediatric patients typically are poor candidates for traditional prostheses, mainly because fitted prostheses can cost tens of thousands of dollars and need frequent resizing and replacement to keep pace with a child’s growth. By comparison, materials for a 3-D printed prosthesis can cost a few hundred dollars.
“The possibilities with 3-D printing in health care have the power to revolutionize medicine,” said Charles Goldfarb, MD, chief of orthopedic surgery at St. Louis Children’s Hospital, who works closely with patients to determine eligibility for prostheses. “It’s exciting.”
Invaluable feedback

Sydney Kendall received a pink robotic arm seven years after she lost her right arm, just below the elbow, in an accident involving a jet ski, boat and rampant rope at the Lake of the Ozarks in central Missouri. Sydney, who lives in suburban St. Louis, was 6 years old at the time, in kindergarten, and, after having just mastered how to print her name, had to re-learn how to write with her left hand. The stares, pointing, awkward and sometimes rude comments thickened her skin during a life stage often marked by innate innocence.
The robotic arm, humorously named “Pinky,” arrived with fanfare during Sydney’s last year of middle school, in May 2014, when she was 13 and in the eighth grade. Powered by a nine-volt battery, the pink prosthesis used a microchip and motion-detecting sensor on Sydney’s shoulder to activate fingers, including independent thumb movement, restoring her ability to throw a ball or move a computer mouse with her right limb.
News media big and small spotlighted Sydney and her pink prosthesis, which looked both primitive and futuristic, a long plastic tube with five spindly mechanical fingers, novel in its ability to help a child amputee regain hand and arm function.
Sydney’s classmates called her famous.
Designed by three Washington University seniors studying biomedical engineering and in collaboration with Shriners Hospitals for Children St. Louis and School of Medicine physicians such as Goldfarb who provided medical expertise, the pink prosthesis cost approximately $200 in materials and took less than a week to print. “My robotic arm was popular, and it made some things easier,” Sydney said, “but, honestly, I had grown used to doing things with my left hand and sometimes it was easier not to wear it.”
Sydney also found the wire connecting the shoulder sensor to the prosthesis cumbersome and inconvenient.
Neither Sydney, her parents nor the three undergraduate students who initially fabricated the prosthesis expected perfection. Quite the opposite. It was the students’ first attempt at a pediatric robotic arm, and it wasn’t as if a successful prototype existed elsewhere. When the MIS team got involved with the project, the prosthesis impressed the scientists; however, they knew they could make improvements. “We wanted to hear what worked and what did not,” said Dominic (Nick) Thompson Jr., a School of Medicine staff scientist who is leading MIS efforts to create pediatric prostheses. “Our goal is to do whatever it takes, for however long, to help kids.”
Based on the family’s feedback, Thompson and two Washington University biomedical engineering undergraduates working in the MIS lab — Nabeel Chowdhury and Savannah Est — created a second prosthetic arm for Sydney that offered a wider range of wrist movement. Sydney controls its functions through myoelectric technology that uses electrodes to read the surface electrical current generated when her arm muscles contract.
She received her new hand late last summer, just in time for her first day of high school.
The prosthetic boasts fancy monogrammed initials and a blue hue because, Sydney said, “I got tired of everyone thinking pink was my favorite color.” Perhaps an even bigger bonus for the teenager: She can hold a cell phone with the prosthetic hand and type with the other.

Not bad for the lab’s bulky 3-D printer that is two years old and initially cost $2,500.
American engineer and physicist Charles Hull developed 3-D printing — officially called stereolithography — during the 1980s for manufacturing purposes, according to the National Inventors Hall of Fame. However, as technology advanced, materials improved and the cost of both decreased significantly during the past few years, 3-D printing has become the darling of the medical and bioengineering industries.
A 3-D printer works similar to an inkjet printer, Thompson said, but instead of ink printing letters and numbers, a 3-D printer uses spools of plastic filament as “ink.” The plastic is heated and extruded by the 3-D printer to form layers to create 3-D models designed by researchers using computer design software.
Although Sydney’s second prosthesis offered significant improvement in aesthetics and weight, it still had issues. The grip strength of the prosthesis, for example, needed to be stronger to allow Sydney to perform additional activities. “Her feedback is invaluable,” Thompson said, “because it brings us closer to creating a problem-free prosthesis.”
Chowdhury, the biomedical research engineering major, is devising plans for a third prosthesis for Sydney. He plans to earn combined MD/PhD degrees because he wants to specialize in 3-D pediatric prostheses. “The need is great,” said Chowdhury, who envisions the low-cost limbs as options to help disabled children from low-income areas both in the U.S. and abroad.
Work in progress

Living without full use of her hands is normal for Olivia. Although she was born healthy, by four months of age she mysteriously developed a rare autoimmune disease — Infantile Polyarteritis Nodosa/Atypical Kawasaki — that inflamed her blood vessels and caused multiple life-threatening aneurysms. To restore blood flow and prevent infections, School of Medicine surgeons amputated Olivia’s right hand, the fingers from her left hand and part of her right foot.
Almost 5 years old, Olivia walks normally and her foot is unnoticeable with shoes. Her hands, however, proved more challenging. Over the years, she has perfected using her teeth (or her knees) to steady objects, and uses her partial left hand and her right wrist to grasp crayons or drinking cups.
“I do things different than my sisters,” said Olivia, the second youngest of five sisters living in Southern Illinois. “My mom says that’s OK.”
Despite her impressive ability to adapt without hands, surgeons removed part of a bone in her left hand to encourage a squeezing motion. For her right hand, the MIS lab’s Thompson, Chowdhury and Est made Olivia a powdery-blue mechanical prosthesis decorated with dinosaurs and her name in cursive.
A mini-cable system in the mechanical hand operates with the flex of Olivia’s wrist.
“Look at me, look at me,” Olivia shouted in the lab last fall when she received her prosthesis. The brown-haired precocious preschooler practiced one-handed maneuvers such as throwing a foam ball and holding a cup.
Her beaming brightness and obvious self-pride inspired a scientist’s eyes to mist.
But all wasn’t perfect. After a few minutes wearing her prosthetic hand, Olivia dissolved in frustration. Her arm muscles lacked the strength to sustain movement in the mechanical hand. The scientists noted possible modifications for easier, prolonged movement and promised Olivia another hand.
Est bent down toward Olivia’s level and said, “One day, you’ll be able to print your own hand yourself.”

Charting the 3-D frontier
The Minimally Invasive Surgery Biomaterials Lab and the Division of Plastic and Reconstructive Surgery are collaborating on a growing list of 3-D printing innovations.
“There is tremendous excitement at Washington University and other universities about devising medical applications for 3-D printing,” said L. Michael Brunt, MD, chair of the MIS lab and a professor of surgery. “Hardly a day goes by that I don’t hear of something new.”
Two years ago, the lab became involved in 3-D printing to design and fabricate hernia surgical mesh. As interest grew, so did the opportunities.
MIS scientists have ventured into creating plastic organs such as kidneys and uteruses for surgical training tools as well as developing techniques for bio-printing, in which living cells are used to form structures.
Anatomical models printed directly from CT scans allow physicians to evaluate patients with extraordinary precision, said Albert S. Woo, MD, associate professor in plastic and reconstructive surgery, who is leading many of the university’s innovations in 3-D printing. As director of the Cleft Palate and Craniofacial Institute at St. Louis Children’s Hospital, Woo can correct facial deformities using parts produced on his department’s 3-D printer.
Another benefit is the potential for reduced costs. Traditional robotic limbs can cost between $50,000 to $70,000. Materials for a 3-D prosthesis hover closer to $200. But price comparisons can be misleading: Pediatric limbs cost a few hundred dollars in materials but that doesn’t include scientists’ labor or capital investments, with some 3-D printers running as high as $350,000.
The medical school has only a few 3-D printers; both Brunt and Woo emphasized the need for more to stay at the forefront. “Three-dimensional printing in the medical field is in its infancy,” Woo said. “It’s exploding with opportunities and transforming health care.”
Published in the Winter 2015-16 issue


