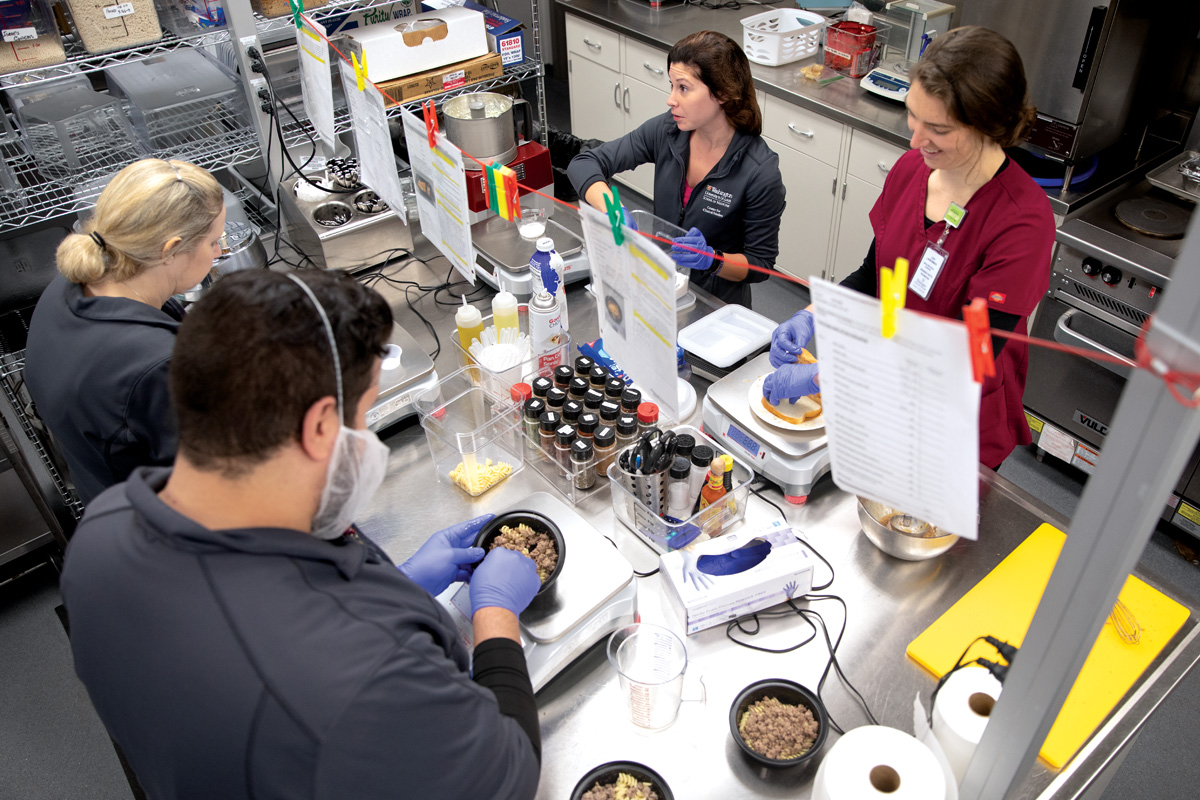
Staff members in a special metabolic kitchen prepare meals for patients enrolled in a diet and metabolism study.
At nearly 250 pounds, Linda DeCosta had tried everything — and failed — to lose weight: prescription drugs, exercise programs, dieting. She had even considered bariatric surgery, but insurance wouldn’t cover it.
“I was almost starving myself,” DeCosta said. “Our family doesn’t eat out a lot. I don’t cook a lot of fried foods. I didn’t know what I was doing wrong.”
Diagnosed with asthma and high blood pressure, her health was suffering. Even the short walk to the bus stop was a struggle.
By the time DeCosta saw the recruitment email for an obesity study looking at metabolism and diet, she had about given up. Motivated by her husband and three children, she decided to enroll. “I figured I won’t be long for this world unless I do something to change this.”
Intensive effort
“Obesity is a major public health problem,” said Samuel Klein, MD, the study’s principal investigator. “It’s abnormal to be lean in this country.”
Klein, the William H. Danforth Professor of Medicine and Nutritional Science, is an internationally renowned expert with more than 30 years of experience studying nutrition, metabolism, obesity and weight loss.
Obesity is linked to a slew of metabolic problems, such as high blood triglycerides, high blood pressure and insulin resistance. Many people with obesity develop chronic conditions such as diabetes, heart disease, fatty liver disease, arthritis, cancer and lung disease.
“Obesity is caused by eating more calories than you expend over a long period of time and storing those excess calories as body fat; excess body fat causes dysfunction in nearly every organ system in the body,” said Klein, who also directs the Center for Human Nutrition at Washington University.

Samuel Klein, MD, (right) watches as Adewole Okunade, PhD, performs a chromatography analysis of blood plasma. Klein’s lab studies nutrition and metabolism in health and disease.
Klein’s research program combines basic and clinical science to examine multiple organ systems simultaneously. Because obesity affects biological function in so many different organs, his group is one of the most collaborative on campus — joining together molecular biologists, physiologists, endocrinologists, cardiologists, immunologists, neurologists, radiologists and psychologists. Nearly 50 clinicians, researchers, technicians, nurses and recruiters collaborate on the team. (See a list of primary collaborators below.)
“To address the complex issues of obesity, you need to conduct research that involves a multi-organ system approach, which requires collaboration among investigators with different expertise,” Klein said. “This kind of research is possible at Washington University because of the collegiality of our faculty and breadth of scientific expertise. I am fortunate to be able to work with so many talented people.”
Losing weight comes down to simple math: people must burn more calories than they consume, so that their bodies use the excess fat as fuel. But it’s not as easy as it sounds, Klein said, because weight loss is influenced by many complex factors, including genetics, birth weight, brain chemicals, cultural and work environment, food availability and marketing, physical activity, stress and the pleasure of eating.
For a person who is obese and consuming 3,000 calories a day, that may mean cutting daily intake to 1,500 calories indefinitely. “How do you get people to eat fewer calories than they normally consume and maintain that low-calorie intake for the rest of their lives? Weight loss maintenance is the Achilles’ heel of weight management,” Klein said.
Also, eating a healthy diet is complicated because different people respond differently to the same food. A serving of potato chips may cause blood sugar to spike in one person, and not another. There is likely no “one-size-fits-all diet.” While the total calories consumed still matters, the composition of those calories may need to vary by individual. This is why personalizing nutrition is the logical next step in fighting obesity and its complications, Klein said. But more research is needed before useful recommendations can be made.
Approximately 10% of those who are obese do not develop metabolic abnormalities. Klein is seeking to understand why some people with obesity are protected from the adverse health effects of excessive body fat. In one study, Klein found that people with metabolically healthy obesity remained healthy even after gaining 6% body weight, whereas those who already had metabolic problems got worse.
The metabolically healthy participants were able to store fat in a healthier way, without impairing their metabolism, unlike in the metabolically unhealthy individuals.
Klein’s current diet and metabolism study is comparing three groups: metabolically healthy people who are lean; metabolically healthy people with obesity; and metabolically unhealthy people with obesity (those with issues such as insulin resistance, high liver fat and high blood triglycerides).
Klein and his collaborators will follow these individuals for several years, particularly those who are obese and metabolically normal, to see if their metabolism remains normal.
The metabolically unhealthy individuals with obesity are randomized to follow one of three popular diets: the low-carb ketogenic or “Keto” diet; the Mediterranean diet, emphasizing fruits and vegetables, whole grains and fish; or a very low-fat, plant-based diet. The plan is to see if these diets have different effects on metabolic and health outcomes.
This research is labor-intensive and involves a team of skilled research coordinators, research nurses and nurse practitioners, dietitians and recruiters. Every week, staff members working in a special metabolic kitchen at the Medical Center’s Clinical and Translational Research Unit carefully plan, prepare and package meals for the metabolically unhealthy participants.

Liquid nitrogen is used to preserve a fat biopsy sample from a study participant. Klein’s group studies the role of fat, a highly metabolically active organ, in obesity.
The diet phase of the study lasts over a year and requires a big commitment from participants, who undergo weekly visits with occasional overnight stays. Tests include assessing insulin action; examining cell metabolism and inflammation from fat and muscle biopsies; measuring body fat content and distribution, as well as brain function through MRI and PET scans; studying the gut microbiome from stool samples; profiling the blood’s metabolites over 24 hours and assessing cardiorespiratory fitness.
Following individuals for long time periods with controlled dietary intake, evaluating biological function in multiple organs, and involving so many collaborators is unique in the nutritional research field.
“Sam Klein is one of the finest clinical and translational investigators in the country, and has built a unique, multidisciplinary obesity research program at Washington University,” said David Brenner, MD, vice chancellor for health sciences at the University of California, San Diego, where Klein has a joint appointment. “He has made seminal contributions to our understanding of the mechanisms responsible for the metabolic abnormalities associated with obesity and the profound therapeutic effects of decreasing body fat in people with obesity.”
This kind of intensive research is also costly. “Sophisticated translational research conducted in people is expensive and requires substantial resources and personnel,” Klein said. “We are fortunate that Washington University has made the commitment to advance this kind of translational research that begins in cell systems but must ultimately lead to costly but necessary human studies.”
Philanthropy is also crucial, he adds, as government agencies do not provide adequate funding for expensive clinical research. The Pershing Square Foundation has made a commitment to advancing research in obesity and funded the study looking at diet and metabolism. Klein also receives funding from other private organizations, including the Robert C. and Veronica Atkins Foundation. In 2003, Klein led the first randomized, controlled trial demonstrating that the Atkins diet produces greater short-term weight loss than conventional diets in those with obesity.
A broad range of research
One-third of U.S. adults and nearly three-quarters of people with obesity have nonalcoholic fatty liver disease, defined as an increase in liver triglycerides, which can progress to cirrhosis and is a leading cause of liver transplantation. Klein’s group is examining the connection between excess fat in the liver and the metabolic abnormalities associated with liver fat accumulation.
Once considered to be an inert tissue, fat is now known to be a highly active organ that secretes proteins and lipids, affecting metabolic function in other organs. To assess fat distribution in the liver and around internal organs, the Center for Clinical Imaging Research assists with MRI scans. Pear-shaped people with fat accumulation in the lower body tend to have fewer metabolic abnormalities than apple-shaped individuals, who carry the majority of their fat in their abdomens. Klein’s group is trying to understand why these differences occur.
To study the growth of fat cells, participants in some of Klein’s studies drink heavy water containing deuterium, an isotope that is twice as heavy as hydrogen. Researchers track the heavy water molecules as they are incorporated into newly made fat cells and into fat cell lipids. This allows the team to evaluate the rate at which new fat cells are made and the importance of fat cell dynamics in regulating metabolic health.
Metabolically abnormal individuals with obesity tend to have more inflammation in their fat tissue than people with obesity who are metabolically healthy. This chronic inflammation is believed to increase the risk of cardiovascular disease and diabetes. Immunologists are looking at fat tissue gene expression and tracking inflammatory cells to understand how inflammation in obesity contributes to chronic diseases.
In people with obesity, the structure and function of certain brain areas differ from people who are lean. And people with obesity and insulin resistance are at increased risk of developing Alzheimer’s disease. Radiologists and psychologists are using functional MRI and PET scanning to study the effects of diet and weight loss on brain structure and the pleasure-inducing dopamine response to food.
As obesity is known to increase heart disease risk, Klein is partnering with cardiologists to look at the health of the blood vessels, as well as the effects of diet on the heart. In collaboration with neurologists, he is also looking at the link between sleep deprivation and sleep quality on body metabolism.
One of Klein’s most seminal findings provides hope for those struggling with weight loss: Losing even 5% of one’s body weight can significantly improve metabolic health. “Moderate weight loss is achievable in many people and is clinically important,” Klein said. “It is important to realize that obesity is a chronic, lifelong disease, so helping patients make small, progressive changes in eating behavior for life is the goal.”
How did we get here?
Unhealthy lifestyle behaviors are the underlying reason for more than half of chronic diseases, such as obesity, diabetes, heart disease and cancer, Klein points out. But willpower, he said, is often not the issue and cannot solve this problem.
“Many highly motivated people who are obese are successful in their professional lives, but they are unable to make the lifestyle changes needed to lose weight and maintain that loss,” he said.
The human race has undergone dramatic changes in lifestyle in a very short time, Klein said. We evolved to avoid starvation by storing the excess calories we consume as fat. But we no longer have to burn energy to find food — we have easy access to a large variety of palatable foods and we have developed many labor-saving devices that contribute to a sedentary lifestyle.
It is now very easy to consume more calories than we need to maintain a healthy weight. “Within a blink of time in Earth’s history, modern society has completely overcome our evolutionary biology,” Klein said. “We have not adequately adapted to this dramatic change in our environment.” The genes once meant to help us survive are now working against us, he added.
Primary care changes
When agreeing to participate in the study, DeCosta figured she would end up in the metabolically normal obese group. After all, her yearly blood work had never revealed elevated blood glucose or blood lipid levels. Klein’s screening showed otherwise.
“I found out I had a predisposition for type 2 diabetes and I was showing signs of fatty liver disease,” DeCosta said. By not doing more in-depth testing, DeCosta said she felt primary care doctors are doing patients a disservice.
Most primary care physicians rely on an A1C test, an indicator of blood glucose levels over time, to determine a patient’s risk of developing diabetes. A better predictor is an oral glucose tolerance test, where the patient drinks a glucose solution and has a blood test two hours later. While not costly, the test is time-consuming and not often prescribed.

Gordon Smith, PhD, measures study participant Linda DeCosta’s resting metabolic rate. DeCosta is participating in one of Klein’s diet and metabolism studies.
Doctors need to become more involved in preventing excessive weight gain and initiating effective obesity strategies for their patients, Klein said. This is where things like medication, tailored diets and even bariatric surgery can come in.
“Less than 2% of patients who are eligible for prescription weight-loss drugs actually receive them,” Klein said. Bariatric surgery is the most effective available therapy for treating obesity and its complications but it is infrequently recommended by doctors.
Ultimately, we need more research to better understand why obesity causes so many diseases and how we can individualize diet therapy for each patient to get the best health outcomes.
After three months on the Keto diet, DeCosta is down more than 30 pounds.
DeCosta says she is now losing weight for herself. Recently, on her way to catch the bus to one of her study visits, she realized she was no longer out of breath.
Interested in becoming a study participant? Call 314-273-0300 or 314-747-2627 or email ashley.roberts@wustl.edu or j.sonnenschein@wustl.edu.
Gaia Remerowski is a senior content strategist in Medical Public Affairs.

A team effort
Klein leads one of the most collaborative groups on the Medical Campus and works with numerous researchers.
- Nada Abumrad, PhD
Molecular analysis of fat tissue (fat) - Scott Beeman, PhD
Fat oxygenation (fat) - Kevin Black, MD
Brain dopamine in obesity (brain) - Todd Cade
Obesity in pregnancy (physical activity) - Marco Colonna, PhD
Immune cells in fat tissue (immune system) - Vincenza Cifarelli, PhD
Lipidema (fat) - Victor Davila-Roman, MD
Heart disease and obesity (heart) - Julia Dunn, MD
Pleasure response in the brain (brain) - Chris Eagon, MD
Bariatric surgery (surgery) - Shaina Eckhouse, MD
Bariatric surgery (surgery) - Sarah Eisenstein, PhD
Brain dopamine in obesity (brain) - Sarah Farabi, RN, PhD
Obesity in pregnancy (metabolism) - Brian Finck, PhD
Liver cellular metabolism (liver) - Anja Fuchs, PhD
Immune cells in fat tissue (immune system) - Robert Gropler, MD
Cardiovascular imaging in obesity (heart)
- Debra Haire-Joshu, PhD
Maternal obesity interventions (public health)
- Tamara Hershey, PhD
Brain dopamine obesity (brain) - Shinchiro Imai, MD, PhD
NAD biology (metabolism) - Brandon Kayser, PhD
Metabolomics (metabolism) - Brendan Lucey, MD
Sleep extension and metabolic health (sleep) - Bettina Mittendorfer, PhD
Metabolism and obesity (metabolism) - Bruce Patterson, PhD
Mathematical modeling of metabolic pathways (metabolism) - Cyrus Raji, MD, PhD
Brain volume and connectivity (brain) - Dominic Reeds, MD
Diabetes (metabolism) - Dimitri Samovski, PhD
Exosomes (fat) - Kenneth Schechtman, PhD
Statistical analyses (biostatistics) - Joel Schilling, MD, PhD
Immune cells in the liver (immunology) - Gordon Smith, PhD
Metabolism and obesity (metabolism) - Richard Stein, PhD
Behavioral education (psychology) - Jun Yoshino, MD, PhD
Molecular analysis of fat and muscle tissue (fat) - Mihoko Yoshino, MD, PhD
Metabolism and obesity (metabolism)
Published in the Autumn 2019 issue